Incorrectly Mixed Cement in Kyphoplasty
Understanding Kyphoplasty and Bone Cement
Kyphoplasty is a minimally invasive spinal surgery used to treat compression fractures (often caused by osteoporosis or trauma). In a kyphoplasty, the surgeon inserts a needle into the fractured vertebra and uses an inflatable balloon to create a cavity. Bone cement (typically an acrylic cement called polymethyl methacrylate, or PMMA) is then injected into the cavity to stabilize the bone. The cement hardens quickly, effectively acting as an “internal cast” that restores strength to the collapsed vertebra and alleviates pain by preventing the fractured pieces from moving. In short, the cement holds the broken bone together from the inside, allowing patients to regain mobility and reduce their pain.
Once mixed, the cement goes through phases – starting thin and gradually thickening. It should not be injected while it’s too liquid. Surgeons are trained to wait until the cement becomes a toothpaste-like or paste consistency before injection. Injecting cement that is too runny increases the risk that it will leak out of the bone into surrounding areas or veins. In a proper kyphoplasty, the surgeon uses continuous live X-ray (fluoroscopy) to monitor cement injection and ensure it stays within the vertebra. The goal is to fill the interior of the bone at a controlled pace and stop before any cement escapes outside the bone.
Why does proper mixing matter? If the cement mixture is incorrect or injected at the wrong time, it may not harden as intended or may flow where it shouldn’t. Cement that is too thin (low viscosity) can seep through cracks in the bone or venous channels. On the other hand, cement that is too thick or setting too fast might not distribute evenly, requiring higher pressure to inject – which can also cause leaks or other damage. In summary, kyphoplasty relies on both the right material and the right technique: the bone cement must be prepared and handled with precision. When these standards aren’t met, patients can be put in danger.
Cement Embolism and Related Complications
When bone cement is incorrectly mixed or injected improperly, one of the most dangerous outcomes is a cement embolism. An embolism in this context means a fragment of the cement travels into the bloodstream and lodges in a blood vessel, much like a blood clot. How does this happen in a spinal procedure? If the cement is too liquid or injected under too much pressure, it can leak into nearby veins in the spine. From there, the blood can carry bits of cement into larger vessels and up to the lungs or heart. A pulmonary cement embolism occurs when a piece of cement migrates to the lungs and blocks an artery there. This is a very serious complication: if bone cement gets into a vertebral vein, it can travel to the lung and cause an artery obstruction (embolism). In other words, a stray piece of cement can become a life-threatening foreign object in the circulatory system.
Symptoms of a cement embolism can resemble those of a blood clot or stroke. A patient might experience sudden-onset chest pain, shortness of breath, rapid heartbeat, or collapse if a cement fragment lodges in the lungs or heart. For example, one 56-year-old kyphoplasty patient went to the ER after two days of severe chest pain and difficulty breathing, only to discover that a 4-inch piece of bone cement had traveled to his heart. In that case, the cement had leaked out during the procedure, hardened, and then embolized through the bloodstream. The fragment pierced the upper chambers of his heart and even punctured his lung. He required emergency open-heart surgery to remove the cement and repair the damage. This real-world incident illustrates how a cement embolism can pose life-threatening risks, including cardiac perforation, lung damage, or even death. Fortunately, not all cement embolisms are so catastrophic – sometimes small cement particles lodge in peripheral lung areas and cause no symptoms – but any cement embolism is cause for serious concern and close monitoring.
Aside from embolisms, other complications can result from improperly mixed or applied cement in a kyphoplasty:
Cement Leakage and Nerve Injuries: The most common issue is cement extravasation, meaning the cement leaks out of the intended area (the inside of the vertebra). Leaked cement can invade the spinal canal or foramina (where nerve roots exit the spine). If cement presses on the spinal cord or a nerve root, it can cause intense pain, nerve damage, or even paralysis. Patients may experience new or worsening back pain, radiating pain, tingling, numbness, or muscle weakness if nerves are affected. In severe cases, such as cement compressing the cauda equina (the bundle of nerves at the base of the spine), it can cause cauda equina syndrome – a surgical emergency characterized by bowel/bladder dysfunction and leg paralysis.
Spinal Cord Compression: A large cement leak into the central spinal canal can bruise or compress the spinal cord. This is rare but devastating. Paralysis or loss of sensation below the level of the leak can occur if the spinal cord is pinched by hardened cement. Emergency surgery may be needed to remove the excess cement and decompress the spinal cord. Even with surgery, neurological deficits (like weakness or paralysis) might be permanent if the cord was severely injured.
Cardiac and Vascular Complications: In extreme cases, cement can travel to the heart and cause cardiac perforation or arrhythmia. As noted, cement in the heart or major vessels can tear the vessel walls or disrupt blood flow. Patients could suffer a heart attack–like event or cardiac tamponade (pressure on the heart from bleeding) if a chamber of the heart is perforated by cement. There have been fatal reports of cement fragments puncturing the heart or causing uncontrolled bleeding in the chest. Even if not directly in the heart, cement blocking a large pulmonary artery can rapidly strain the heart and lungs, leading to a life-threatening condition.
Other Potential Issues: Cement toxicity and allergic reactions are rare but possible. Bone cement contains chemicals that can cause a drop in blood pressure or other systemic effects if large amounts reach the bloodstream (this is usually transient and monitored by anesthesiologists during the procedure). Infection is a general risk with any surgery, though infection specifically from the cement is uncommon since the cement itself tends to be antibacterial when it hardens. Another recognized issue is adjacent vertebral fractures in the future – the treated bone becomes very rigid, and the level above or below might fracture due to transferred stress. However, whether kyphoplasty significantly increases adjacent fracture risk is still debated.
It’s important to note that many kyphoplasty cement leaks do not cause symptoms – in fact, studies have found small cement leaks happen in a significant percentage of procedures, but most are harmless and only noticed on X-rays. Complications tend to arise when a large leak occurs or the cement travels to a critical area like the spinal cord, heart, or lungs. In one analysis of vertebral augmentation lawsuits, cement leakage into the spinal canal was the single most common allegation, cited in about 45% of malpractice cases studied. This underscores that when a leak does cause harm (like nerve injury), it is often considered a serious deviation from the expected outcome and can lead to legal action.
Medical Malpractice and Liability
Not every complication from a kyphoplasty is the result of malpractice – sometimes bad outcomes occur even when doctors follow the proper standard of care. However, if a patient’s injury was caused by improper mixing or handling of cement that fell below the accepted standard of medical care, it may constitute medical malpractice. Malpractice is essentially medical negligence: it means the healthcare provider did not do what a reasonably careful provider would have done in that situation, and that substandard care caused the patient harm.
So, when does incorrect cement mixing or technique cross the line into negligence? One example would be if the surgeon or assistant failed to wait until the cement was adequately thick and injected it while it was too fluid, causing a preventable leak. Another would be if the provider wasn’t using fluoroscopy imaging properly and missed obvious signs that cement was flowing toward unwanted areas. Kyphoplasty is considered a routine and safe procedure, but terrible outcomes can occur if the surgeon does not follow protocol – for instance, if cement is negligently injected into the wrong location (such as a blood vessel instead of the bone). Proper technique dictates constant monitoring and careful injection; if a doctor skips steps, rushes, or ignores warnings (like cement visibly leaking on the X-ray), that could be a breach of the standard of care.
From a legal standpoint, a plaintiff (injured patient) must prove four key elements in a malpractice case: duty, breach, causation, and damages. In a medical setting, duty is straightforward – the surgeon or hospital owed a duty to treat the patient according to the medical standard of care. The critical questions are breach and causation: did the provider breach the standard of care, and did that breach directly cause the injury? Establishing a breach usually requires an expert medical witness to review the facts. Expert testimony is used to show what a competent surgeon would have done and how the defendant’s actions deviated from that standard. For example, an expert spine surgeon might testify that in a kyphoplasty, no careful doctor would inject cement at such a low viscosity or would have halted the procedure upon seeing cement enter a vein – and that failing to do so was negligence. Causation means linking that mistake to the outcome: the expert must also explain that, but for the negligence, the patient likely would not have been injured (e.g., “Had the cement been properly mixed and injected, it would not have embolized to the lungs and the patient would not have nearly died from a pulmonary embolism”).
Who can be held liable in these situations?
In many cases, the primary liable party is the surgeon or physician who performed the kyphoplasty, since they are responsible for mixing and injecting the cement (often with assistance of a radiology tech or nurse). If an assisting medical professional mixed the cement improperly, the surgical team or hospital may share liability, but typically the lead doctor is accountable for their team’s actions under the doctrine of “captain of the ship” in the OR. The hospital or surgical center might also be liable independently if, for example, they provided faulty equipment (like a defective cement delivery system) or if they allowed an unqualified clinician to perform the procedure. In some cases, even the medical device or bone cement manufacturer can be held liable under product liability law – this would apply if the cement itself was defectively made or marketed.
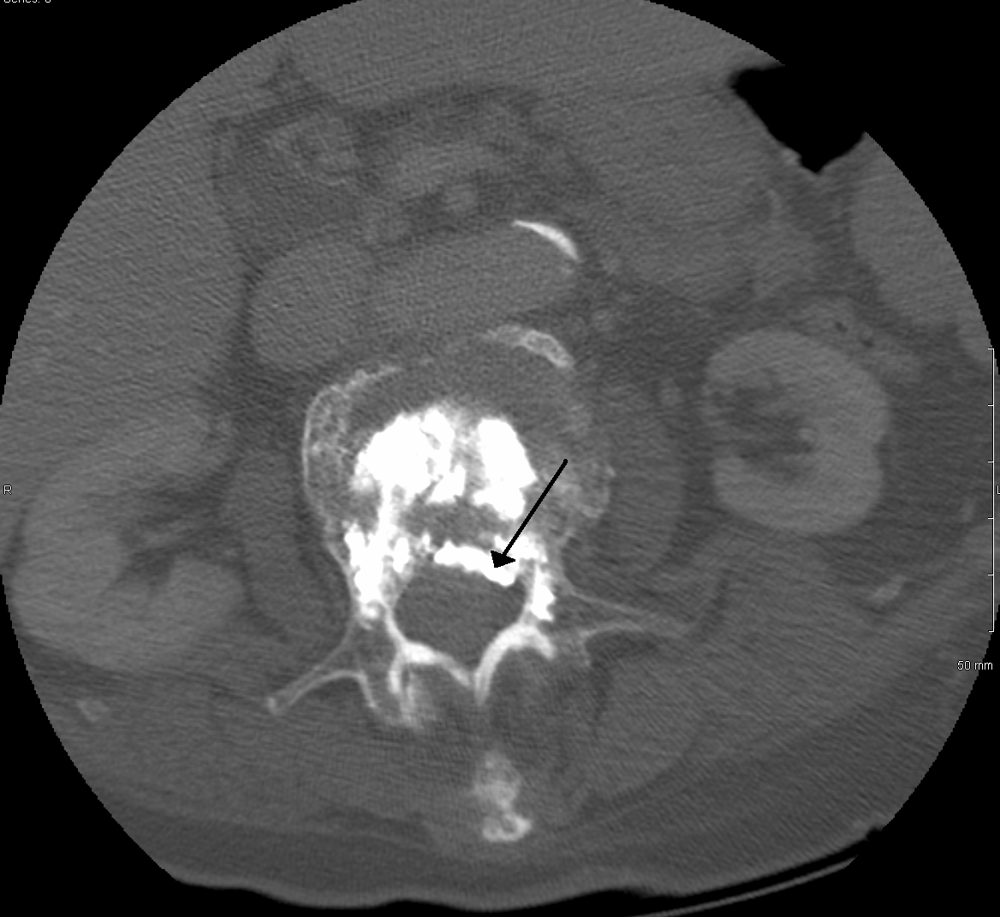
To prove negligence in a case like this, a plaintiff’s legal team will heavily rely on medical records and imaging. The operative report, for example, might document how much cement was used and whether any complications were noted during the procedure. Postoperative X-rays or CT scans can show where the cement ended up. These pieces of evidence, interpreted by expert witnesses, form the backbone of demonstrating a deviation in care.
Legal Options for Affected Patients
If you or a loved one has experienced a serious complication after a kyphoplasty – especially something like a cement embolism, new neurological problems, or other unexpected injuries – it’s important to know you may have legal recourse. Here are steps to take if you suspect medical malpractice in such a situation:
-
Seek appropriate medical care for your complication. Your health comes first. Ensure you get the necessary treatment for any injury (e.g., surgery to remove leaked cement, rehabilitation for nerve damage, etc.). Not only is this crucial for your well-being, but it also documents the extent of harm caused by the initial procedure.
-
Obtain your medical records. Request copies of all relevant records, including the operative report from the kyphoplasty, hospital records, imaging studies (X-rays, CT/MRI scans), and follow-up notes. These records will be critical for any review of what went wrong. They can reveal, for example, if the operative note mentions “cement leakage” or if fluoroscopy images showed abnormal cement flow.
-
Consult a qualified medical malpractice attorney. An experienced attorney can evaluate the facts of your case and advise if a malpractice claim is viable. Many malpractice lawyers offer free initial consultations. Given the complexity of spinal surgery cases, it’s wise to find an attorney (or firm) with experience in surgical or orthopedic malpractice. They may also have on-hand medical experts (or will hire an outside expert) to review your records. Expert review is essential – a spine surgeon or interventional radiologist expert will look at your case and determine if the kyphoplasty was performed below the accepted standard of care.
-
Do not delay in seeking legal advice. Medical malpractice claims are subject to a statute of limitations, which varies by state (often around two years from the date of injury or discovery of injury, with some exceptions). If you wait too long, you could be barred from filing a lawsuit. Additionally, early action helps preserve evidence. Over time, witnesses may forget details, or records may be harder to obtain. It’s best to start the process as soon as you suspect that a serious mistake occurred.
-
Keep notes of your experience and losses. It can be helpful to maintain a journal of the symptoms you suffered after the procedure, the treatments and surgeries you’ve undergone to address the complications, and how this has impacted your daily life. Also keep track of expenses related to the injury (medical bills, travel for treatment, lost work days, etc.). This information will be useful in building your case and demonstrating your damages.
When you meet with an attorney, they will usually help you understand whether the outcome of your kyphoplasty was a known risk or truly the result of negligence. As mentioned, not every cement leak is malpractice – the key question is whether the surgeon breached the standard of care. A good lawyer will often arrange for an independent medical expert to review the case. If the expert concludes that the surgeon did something wrong (or failed to do something important) that caused your injury, the attorney may proceed with a claim.
Proving a malpractice claim involves showing evidence of negligence (such as testimony that the cement was mixed improperly or injected negligently) and drawing a clear line from that negligence to your injury. This typically culminates in either a negotiated settlement with the providers (or their insurance) or, if no settlement is reached, a lawsuit filed in court. Keep in mind that malpractice cases can be complex and costly to litigate, often requiring depositions of medical staff and dueling testimony from experts. However, many such cases do settle before trial if the evidence of negligence is strong.
If your case is successful – whether via settlement or a court verdict – you may be entitled to compensation for the harm you suffered. In a medical malpractice lawsuit, patients can recover both economic and non-economic damages. Economic damages compensate you for financial losses caused by the injury. This includes medical expenses (such as the cost of additional surgeries, hospital stays, medications, rehabilitation, and future medical care you’ll need), lost wages for time you were unable to work, and even loss of earning capacity if the injury limits your ability to work in the future. Non-economic damages address the more intangible losses – most significantly, pain and suffering. Suffering can be physical (chronic pain, disability) as well as mental. Many patients endure significant emotional distress, depression, or loss of enjoyment of life due to a spinal injury or major health scare, and they can seek compensation for these psychological impacts. For example, if you now struggle with mobility or can no longer partake in activities you loved, those are real harms resulting from the malpractice. In cases of egregious wrongdoing, punitive damages might also be sought to punish the wrongdoer, though these are rare in medical cases and often capped by law. The specific damages available will depend on your jurisdiction and the particulars of your case, but an attorney will help ensure that any lawsuit fully accounts for all the ways the malpractice affected your life.
Conclusion and Next Steps
Undergoing a kyphoplasty is supposed to help a patient, not hurt them. While the procedure has a good safety record overall, the misuse or improper mixing of bone cement during the surgery can lead to devastating complications that no patient expects – cement in the lungs or heart, paralysis from spinal cord compression, and other life-altering injuries. The law recognizes that patients have the right to safe treatment and to be free from avoidable errors. Thus, when preventable mistakes occur due to a provider’s negligence, patients have the right to seek accountability and compensation through a malpractice claim.
If you suffered a complication that you suspect was caused by a medical error in a kyphoplasty or vertebroplasty, don’t hesitate to get a professional opinion – both medical and legal. Start by consulting with another trusted doctor to understand what went wrong medically. Then, consult a medical malpractice attorney to understand your legal options. A lawyer can help determine if your outcome was a known risk (that was properly managed) or if it stemmed from substandard care. Remember, pursuing a legal case not only could provide you with financial relief for your losses, but it can also drive improvements in medical practices by holding providers accountable. Patients injured by negligence deserve a voice and compensation for their suffering.