Lost Income Benefits Guide for Injured Workers

Workers’ compensation covers the 100% of the cost of necessary medical treatment, and injured workers should not have to pay out of pocket. However, disputes over coverage can arise.
The Panel of Physicians
The form pictured below is called a “panel of physicians”.
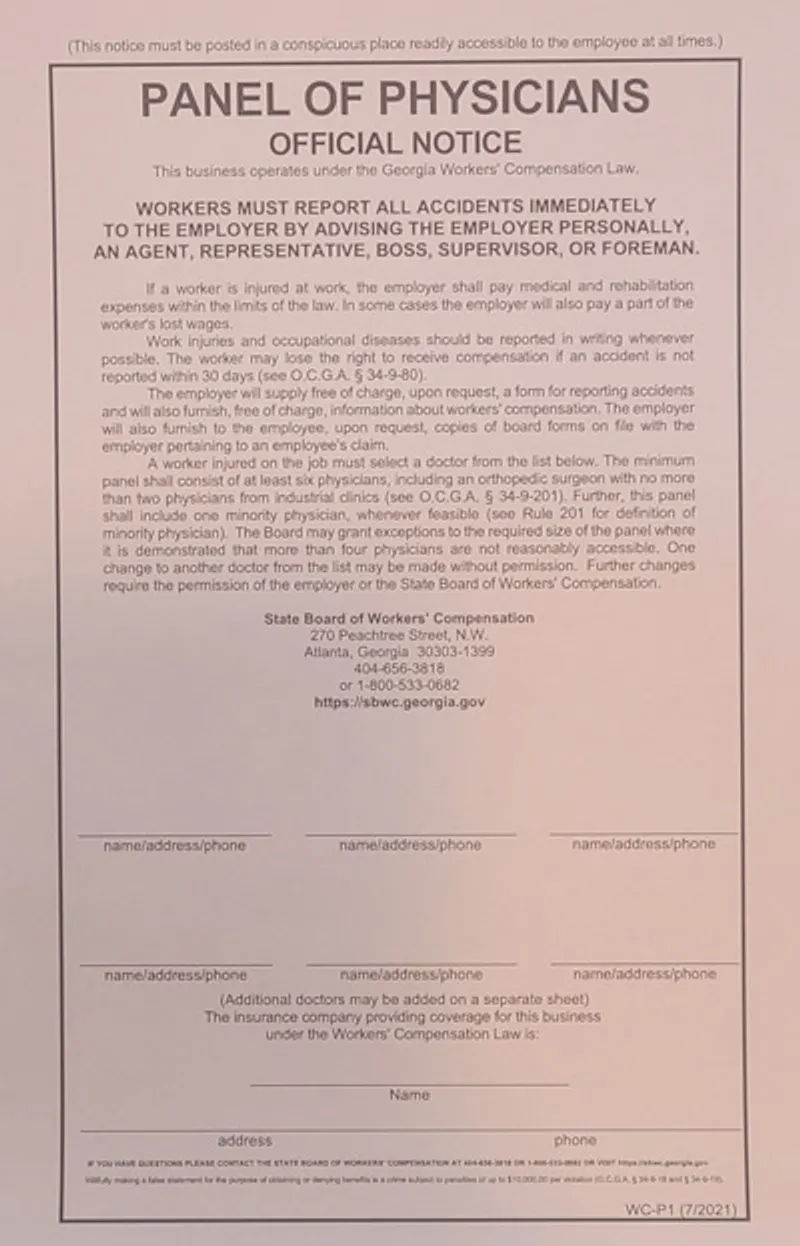
This list of doctors is required to be posted in the workplace and this list must be accessible to you. You’re entitled to choose any doctor that you want off of this list.
Choosing The “Authorized Treating Physician”
The doctor you select from the panel of physicians will become your “authorized treating physician.” This is the doctor who will be responsible for your medical care and treatment.
An authorized treating physician (ATP) is a medical professional designated to provide care for an employee’s work-related injuries under the Workers’ Compensation Act. The ATP plays a central role in the treatment and management of the employee’s medical needs and recovery. Their responsibilities include:
- Providing Medical Treatment: The ATP is responsible for delivering reasonable and necessary medical treatment to grant relief, effect a cure, or restore the employee to suitable employment. This includes addressing the employee’s work-related injuries and ensuring the treatment aligns with the requirements of O.C.G.A. §34-9-200(a).
- Referring to Specialists: The ATP has the authority to refer the employee to other specialized medical services or treatments as required by the nature of the injury, without needing prior authorization from the Board.
- Determining Work Restrictions: The ATP may assess the employee’s ability to work and provide recommendations regarding work restrictions or limitations. This can include determining whether the employee is capable of returning to work with or without restrictions.
- Treatment Plan Development: The ATP is responsible for developing and implementing a treatment plan tailored to the employee’s specific injuries. This plan may include consultations, therapies, medications, or other interventions necessary for recovery.
- Medical Documentation: The ATP must maintain accurate and detailed medical records, which may be used in workers’ compensation proceedings. These records are critical for determining the appropriateness of treatment and the employee’s progress
- If disputes arise regarding the reasonableness, necessity, or relatedness of medical treatment, the ATP’s opinions and records often play a pivotal role in resolving such disputes.
Who you choose as your authorized treating physician is very important. This initial decision can have a significant impact on your recovery and the benefits you receive.
Doctors To Avoid
Some medical providers have a BIG conflict of interest regarding YOUR medical care. They focus on workers’ compensation insurance and get hundreds of patients directly referred to them from the workers compensation insurance companies. One of the biggest mistakes we see is going to an “occupational clinic” or “industrial clinic.” These companies know they will get sent more injured workers if they help the insurance company instead of you. Some examples of industrial clinics to avoid are:
- Concentra
- Caduceus
- Nova
This is not a compelete list and you need to be very careful about who you choose to treat your injury.
Sometimes, a company will not offer to show the list to injured workers or tell you that have to go to a specific doctor. If this happens, you should immediately contact a workers’ compensation attorney.
Industrial clinics will often refuse to put you on a “no work” status, even if you have a serious injury. If you search their website, you may even find them bragging in their marketing materials about how much money they save the insurance company by not taking injured workers out of work.
This is a clear conflict of interest and you should avoid these clinics at all costs.
What if the panel of physicians is invalid?
If a panel of physicians is invalid, you are entitled to choose your own doctor.
The list must have at least six doctors on it and one of the doctors must be an orthopedic doctor. And, the list cannot contain more than two industrial clinics (for example, Concentra). If your employer either does not have a list or their list is invalid (for example, it has less than six doctors) then your employer is not allowed to limit your choice of doctors. You can choose any doctor that you want and workers compensation must pay for it.
It is not uncommon for employers to have an invalid panel of physicians. For example there might not be enough doctors, the panel might not have an orthopedic doctor, or the doctors on the panel are out of business. The panel must also be posted at a prominent location on the wall at your workplace. Usually it will be posted in a office or a break room. Use your phone to take a picture of the panel.
However, usually the employer and insurance company do not want to acknowledge that their panel is not valid. They will resist letting you choose your own doctor (in clear violation of the law). If your employer’s panel of physicians is invalid, you usually need to get a workers compensation lawyer involved to help you pick your own doctor.
Example

After injuring his hand on the production line, Robert checks the workplace’s posted list of approved doctors. He quickly notices that the list only contains five names and does not include an orthopedic specialist, as required by law. Determined to protect his rights, Robert takes a picture of the panel to document its invalidity. Since the list fails to meet the state requirements, Robert is able to select his own doctor for treatment, ensuring he receives the best possible care for his injury.
Other Ways To Get A New Doctor
The State Board of Workers’ Compensation has the authority to order a change in physician to another doctor. This authority is granted under O.C.G.A. § 34-9-200(b), which states that upon the request of an employee, employer, or on its own motion, the Board may order a change of physician or treatment. The decision is made based on the Board’s judgment and discretion
You will need the assistance of a workers’ compensation attorney to file a request with the Board. The Board considers a non-exclusive list of factors outlined in Board Rule 200(b)(2) when deciding whether to grant a change of physician. These factors include, but are not limited to:
- Proximity of the physician’s office to the employee’s residence.
- Accessibility of the physician to the employee.
- Necessity for specialized medical care.
- Duration of treatment without appreciable improvement.
- Referral by an authorized treating physician.
- Current physician indicating they have nothing more to offer.
- Excessive or redundant performance of medical procedures.
- Employee’s confidence in the treating physician.
Although the Board has the authority to order a change of physician, it is not obligated to do so. The decision is made on a case-by-case basis, considering the specific circumstances and evidence presented by the parties involved. It is often difficult to get the Board to order a change of physician, so it is important to have a workers’ compensation attorney who is experienced in this area. This process can also take many months if the employer objects to the change, so it is important to be patient.
A change of physician can also occur by mutual agreement between the employee and the employer/insurer. This agreement does not require prior authorization from the Board. Once the parties agree to a change of physician, they should document this agreement using Form WC-200a. This form is used to record the consent of the parties and the details of the new authorized treating physician.
Emeregency Room Treatments
There is an exception for emergency treatment. Sometimes insurance companies try to avoid paying emergency room bills (arguing that the emergency medical provider is not on their panel). In a true emergency, workers compensation insurance is required to cover the treatment.
Drug Testing After a Workplace Injury
Some occupational medicine clinics drug test every injured worker after every accident. If a drug test shows a positive for a substance like marijuana, the insurance company may deny your claim. If you are concerned about this, you should contact a workers’ compensation attorney as soon as possible.
Right To A Second Opinion
You may have the right to a second opinion paid for by your employer.
Under O.C.G.A. § 34-9-202(e), an employee who has sustained an accepted compensable injury and has received income benefits has the right to one examination by a physician of their choice, paid for by the employer, within 120 days of receiving those benefits.
If you have not received income benefits within the last 120 days, you are not entitled to a second opinion. However, you may still pay for a second opinion out of your own pocket.
Right To A Switch Doctors
If you are unsatisfied with your current doctor, you may have the right to switch to another doctor on the panel of physicians. However, you may only switch doctors once without permission.
Denied Medical Benefits
It is not uncommon for insurance companies to deny medical treatment as unnecessary. The employer is required to file a Form WC-3 (Notice to Controvert) if they deny treatment as unnecessary and you should receive a copy of this form.
Medical treatment must be “reasonably required” and appear “likely to effect a cure, give relief, or restore the worker to suitable employment” under O.C.G.A. § 34-9-200(a). If treatment does not meet these criteria, it may be deemed unnecessary. For instance, an insurance company may claim additional surgery would not benefit the employee and might worsen their condition. The insurance company may also try to claim that the reccomended treatment is not related to your work injury.
If you are denied medical treatment, you should contact a workers’ compensation attorney immediately. You may be able to get the insurance company to pay for the treatment by filing a claim with the Georgia State Board of Workers’ Compensation.
The employee or their representative can file a Form WC-14 with the State Board of Workers’ Compensation to request a hearing to resolve the dispute. This is necessary when there is a disagreement over whether the medical treatment is reasonable, necessary, or related to the compensable injury.
Example
John, a manufacturing worker, injured his lower back while on the job and was left with chronic pain. His treating physician, Dr. Carter, recommended the implantation of a spinal cord stimulator to relieve his pain and help him return to work.
However, the insurance company denied the treatment as unnecessary, arguing that it wouldn’t effectively restore him to suitable employment. Following this denial, John’s employer filed a Form WC-3 (Notice to Controvert), and John received a copy of the notice.
Recognizing the severity of his condition, John immediately reached out to a workers’ compensation attorney, who filed a claim with the Georgia State Board of Workers’ Compensation. At the hearing, the administrative law judge reviewed the medical evidence and Dr. Carter’s recommendation, ultimately ruling that the spinal cord stimulator was both reasonable and necessary. The judge ordered the insurance company to authorize and pay for the treatment, ensuring that John received the care he needed.
Delayed Approval of Medical Treatment
Most doctors want pre-approval from the insurance company before they provide treatment. This is called “prior authorization.” If the insurance company does not approve the treatment, the doctor will not provide it. This can lead to delays in treatment and can be very frustrating for injured workers. If you are having trouble getting your doctor to provide treatment, you should contact a workers’ compensation attorney.
A workers comp attorney can help speed up approvals by filing a “WC-PMT” with the Board. When an ATP recommends medical treatment or testing, and the Employer/Insurer has been provided documentation of the recommendation but fails to authorize it within at least five business days, the Employee or their attorney may file a WC-PMT petition. This petition is a request to show cause why the recommended treatment or testing should not be authorized. Upon filing, the Board typically schedules a telephonic show-cause conference with an administrative law judge (ALJ) within five business days of the petition’s filing date. The purpose of this conference is to address the reasons for the delay in authorization.
400 Week Limit On Medical Benefits
The employer/insurer is responsible for covering all reasonable and necessary medical expenses incurred as a result of the treatment provided by the chosen physician, as long as the treatment is related to the compensable injury and meets the standards of being likely to effect a cure, give relief, or restore the worker to suitable employment under O.C.G.A. § 34-9-200(a) However, there is a 400 week limit on medical benefits for non-catastrophic injuries. This means that the insurance company will only pay for medical treatment for 400 weeks (or approximately 7.5 years) after the date of the injury.
If you have a catastrophic injury, there is no limit on medical benefits.
Reimbursement For Travel Expenses
You may be entitled to reimbursement for travel expenses incurred while traveling to and from medical appointments related to your work injury. This includes mileage, parking fees, and tolls. You should keep a record of your travel expenses and submit them to the insurance company for reimbursement.